By Dr. Heather Mastrianno
Meet Olivia
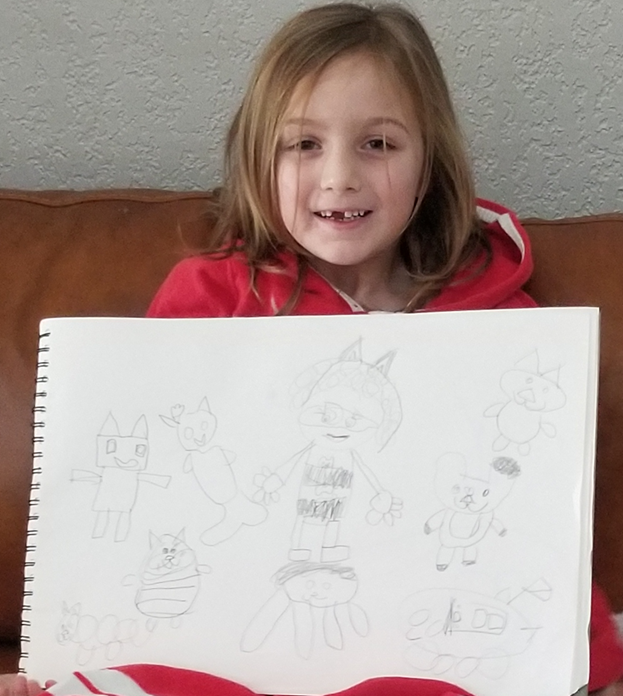
This is a picture of Olivia in December 2021. She just turned 6 years old and started Kindergarten.
Definition and Symptoms of Dystonia
This is what Olivia was experiencing:
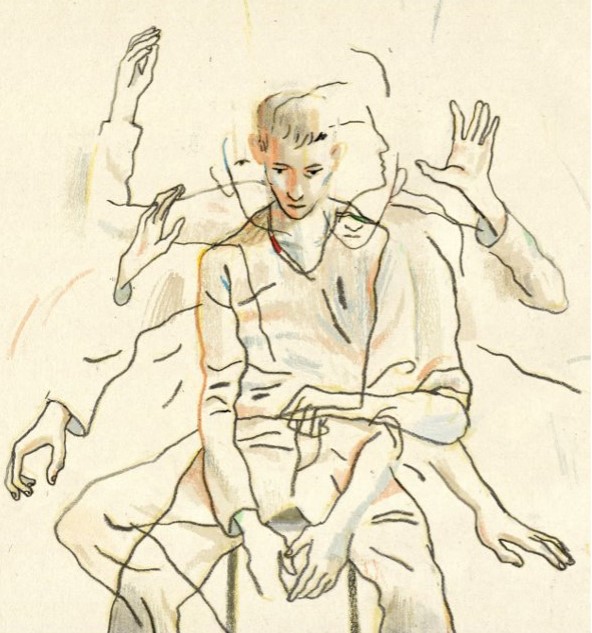
Dystonia is a movement disorder characterized by the involuntary and abnormal co-contraction of opposing muscles. This can cause sustained abnormal postures, twisting, or repetitive movements (Abdo et al., 2010).
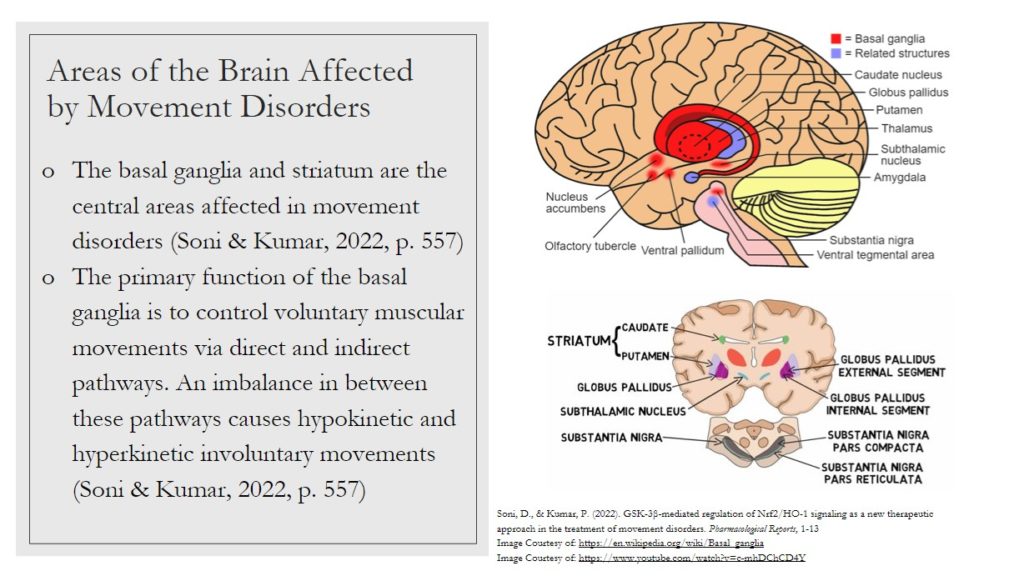
It involves dysfunction within several parts of the brain, including the basal ganglia, cortex, and cerebellum, as well as their connections in the sensorimotor network (McClelland et al., 2021).
References:
-
Abdo, W. F., Van De Warrenburg, B. P., Burn, D. J., Quinn, N. P., & Bloem, B. R. (2010). The clinical approach to movement disorders. Nature Reviews Neurology, 6(1), 29-37.
-
McClelland, V. M., Fischer, P., Foddai, E., Dall’Orso, S., Burdet, E., Brown, P., & Lin, J. P. (2021). EEG measures of sensorimotor processing and their development are abnormal in children with isolated dystonia and dystonic cerebral palsy. NeuroImage: Clinical, 30, 102569.
My first sight of Olivia’s tics:
In December 2021, Olivia began yawning a lot in the evenings. At first, I didn’t think much of it. One evening, she became frustrated and told me:
“Mom, I want to go to bed right now so that I can stop yawning!”
I laughed, kissed her goodnight, and explained that yawning just meant she was tired and needed to sleep, but there was no reason to be upset about it. At the time, I thought her comments were silly and odd.
Looking back now, I realize that was the beginning of the tics.
What is a Movement Disorder?
Movement disorders refer to a group of neurological conditions that affect the nervous system. They cause either increased movements or reduced, slowed movements. These movements may be voluntary or involuntary (Mayo Clinic, n.d.).
Clinical Presentation
Hypokinetic movement disorders refer to akinesia (lack of movement), hypokinesia (reduced movement), and bradykinesia (slow movement).
Hyperkinetic disorders are defined by jerky, excessive movements that may appear alone or alongside non-jerky movements. Learn more here.

Something Might be Wrong…
Our breaking point: Monday, January 3rd, 2022. Olivia was home from school, so my husband and I had to split shifts. That morning, I was home with her. Olivia’s tics had progressed to full mouth opening and closing, over and over, and now her head started twisting too. I tried not to cry when I saw her. I kept thinking:
“How is this happening?! Where did it come from?! Is this permanent?! Is she going to get made fun of?! What will this do to her self-esteem?!”
I tried to call my husband to warn him it had gotten even worse, but before I could say anything other than “it’s not good,” he quickly became worried – he was noticing it too.
I understood. I wanted it to disappear too. I wanted to run from it, to not see it, to hope it was just a dream. The tics at this point were obvious and alarming in frequency. They were happening every 30 seconds to a minute while she was resting or not actively talking or moving. Even when she spoke, as soon as she paused, the tics returned.
As soon as I got to work, my husband called me. He was crying. I had never heard him so distraught. He said,
“Heather, it’s bad. We need to start neurofeedback now.”
I checked the schedule, found an opening, and told him to bring her to the clinic within an hour. He did, and so our neurofeedback journey began.
As all of this was happening, I felt uniquely privileged. I had tools that most others didn’t: a background in and understanding of neurofeedback. I knew it would be the only answer for her because I had seen it work before. I needed to hold onto the belief and knowledge that this could help my child too.
I also knew I needed to record all of this – not just to track my daughter’s progress, but for other mamas and daddies, daughters and sons who didn’t know about this treatment. This was bigger than me. I felt compelled to share our story with others.
Prevalence

This is the statistic category that Olivia fell into:
- 42 million people have been estimated to suffer from some form of movement disorder in the US (Michigan Medicine, n.d).
- The prevalence of tics in school-age children and adolescents can be as high as 21% (Abdo et al., 2010, p. 29).
Other statistics of Dystonia
- The overall prevalence of Parkinson’s disease is 1% in people aged 65-85 years, increasing to 4.3% above the age of 85 years (Abdo et al, 2010, p. 29).
- The overall prevalence of essential tremor is 4% in people aged over 40 years, increasing to 14% in people over 65 years of age (Abdo et al., 2010, p. 29).
Abdo, W. F., Van De Warrenburg, B. P., Burn, D. J., Quinn, N. P., & Bloem, B. R. (2010). The clinical approach to movement disorders. Nature Reviews Neurology, 6(1), 29-37. Movement disorders. Michigan Medicine. (n.d.). Retrieved September 9, 2022, from www.uofmhealth.org
My Next Steps: Google and Facebook Search
Like any frantic parent facing a diagnosis they didn’t understand, I immediately pulled up my computer and started googling. Our pediatrician didn’t want to officially diagnose Olivia with dystonia until we did the placebo trials, but the more I read and watched videos, the clearer her diagnosis became to me.
I quickly joined Facebook groups like “Movement Disorders and Stereotypes in Children” and “Dystonia Support & Awareness.”
I started seeing videos of kids with symptoms similar to Olivia’s, but I wasn’t prepared for everything else I saw: post after post about medications. It made me sick. I didn’t want my child on a bunch of meds. As a psychologist, I deeply understand the value of medication, but my heart broke reading about all the different medication cocktails and suggestions.
What I didn’t see was an answer or a solution that felt right for me or my daughter.
Meanwhile, Olivia’s tics continued to change and worsen. She began yawning throughout the day, especially when she was relaxing or watching TV. The yawns started to look less “natural” and more contorted.
Olivia was experiencing these types of motor tics:
This is a type of hyperkinetic disorder. Unlike myoclonus or chorea, patients with these tics often report a rising feeling of discomfort or an urge (known as a ‘sensory tic’) that is relieved only by performing the movement (Abdo et al., 2010).
It’s also important to note that while tics can sometimes be suppressed, doing so often leads to growing inner tension, resulting in a ‘rebound’ effect where the tics return even more intensely afterward (Abdo et al., 2010).
Abdo, W. F., Van De Warrenburg, B. P., Burn, D. J., Quinn, N. P., & Bloem, B. R. (2010). The clinical approach to movement disorders. Nature Reviews Neurology, 6(1), 29-37. Image Courtesy of: https://www.nytimes.com.
Over the next few weeks, I began reaching out to people I knew. I called my mom to tell her what was happening. Emotionally, I was struggling with seeing my daughter like this. I told my mom how worried I was about what the other kids at school might say or do. I feared Olivia would be made fun of.
My mom’s advice – to start her in yoga and make sure she had a calming environment at home – only made me feel more helpless. I knew that wasn’t going to “fix” it, but I booked her a two-hour massage anyway. It did relax her, but it didn’t change her tics.
In the back of my mind, I kept reminding myself that I had something not many others did: knowledge of and experience with neurofeedback. That gave me hope.
After weeks of reading endless posts about medications, I finally posted in the Movement Disorders groups:
“Looking for anyone who has used neurofeedback for the treatment of tics!”
I got a few likes and a couple of people asked me what neurofeedback was. I felt such frustration and anger – in groups with 881 and 6.9K members, no one seemed to have tried it. I realized that not only did people not use neurofeedback, many didn’t even know it existed.
That moment made me aware of something bigger: I needed to start documenting our experience. I had to pursue what I knew could help my daughter – to give her the best chance, not just for symptom relief, but for real healing.
Trying all the Things
At the beginning of neurofeedback, during the assessment phase, Olivia not only received an EEG evaluation of her brain activity, but we were also advised to have her undergo psychological testing. By having her tested, we could compare areas of her brain that were under- or over-performing with her mental health presentation, including her cognitive abilities.

This was incredibly helpful – it gave us a clear understanding of how she was functioning cognitively and emotionally, and it provided her neurofeedback technician with valuable information for developing her training plan. For example, psychological testing revealed that Olivia has ADHD.
This allowed her technician to choose a protocol that targeted both her tics and her concentration. For us, it was a two-for-one solution and well worth the additional time.
The Otolaryngologist – Ear, Nose and Throat Doctor
To rule out other possible contributing factors, we took Olivia to an ENT to ensure there wasn’t anything in her ears, nose, or throat causing the involuntary movements. The ENT seemed surprised we were there. I explained we were waiting for her neurology appointment, which was booked far in advance, and that we had started neurofeedback while we waited.
He quickly dismissed it, saying, “Whatever, you really just need to take her to a neurologist.” It was horrifying to hear a medical professional brush off neurofeedback like that. I thought about how many other families might have asked him about it and received the same response. It was disheartening for me, and I have a background in this – I can only imagine how hopeless it would feel for someone who didn’t.
The Pediatrician
I also made an appointment with her pediatrician. We asked about a diagnosis for her tics, but she didn’t really know how to respond. She suggested giving Olivia a placebo and telling her it was to treat her facial movements. If that didn’t work, she recommended making an appointment with a neurologist. She offered no clarity or diagnosis.
A neurologist?! That was scary. It was the first time our pediatrician couldn’t help my child.
Trying a Placebo
In the first few weeks of December, we gave Olivia allergy medicine and told her it would help the movements in her face go away. She was so excited to take it, and it broke my heart because I knew I was lying. I didn’t have an answer, and seeing her eagerly ask for the ‘medicine’ or request to take more because of her frustration was gut-wrenching.
She was becoming increasingly embarrassed by the tics, especially when others noticed. It was clear she couldn’t control them, and watching her struggle emotionally with what was happening to her hurt me deeply.
What is Neurofeedback?
Neurofeedback is a technique that makes brain activity perceptible to the senses, allowing individuals to consciously alter it. This is done by recording brain waves with an electroencephalogram (EEG) and presenting that information visually and/or audibly to the client. An EEG is a tool used to detect and record brain wave activity.
During neurofeedback:
-
Brain activity is recorded using sensors and an amplifier.
-
The neurofeedback practitioner or technician then interprets the collected data — including brain activity patterns, clinical questionnaires, and the client’s primary concerns — to create an individualized treatment plan.
Additional information gathered in this process often includes:
-
Relevant medical and mental health history
-
Current medications and dosages
-
Previous traumatic brain injuries (TBIs) or concussions
-
Family history relevant to treatment
Olivia’s Initial Neurofeedback Session

During Olivia’s first neurofeedback session, we completed a six-site assessment of her brain activity. This assessment measured the six main quadrants of her brain to determine how closely her brain waves aligned with normative ranges.
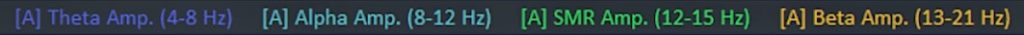
After reviewing the assessment results and discussing our goal of reducing her involuntary motor movements, her neurofeedback technician explained the plan: to target Olivia’s sensory motor cortex, the part of the brain directly involved in bodily movement control. The technician described how they would reward a specific brainwave frequency called Sensory Motor Rhythm (SMR), which falls in the 12–15 Hz range. This frequency is typically associated with both emotional and physical calming.
Our neurofeedback technician positioned an electrode at scalp location CZ (over the sensory motor cortex) to monitor and train the brain activity in that specific area.

What Happened in Olivia’s First Neurofeedback Session
During her session, Olivia watched a movie. The movie would play only when she increased her SMR activity (12–15 Hz), effectively rewarding her brain for producing this calming frequency.
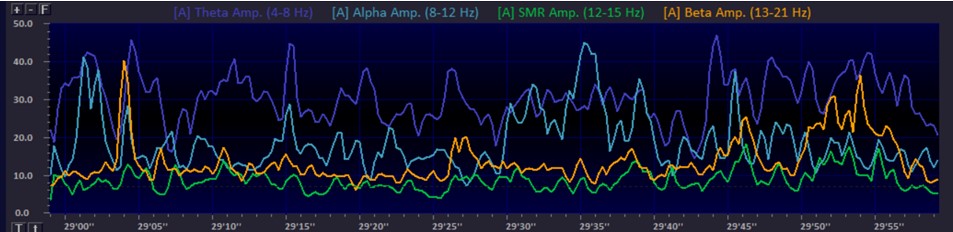
At the end of the session, our technician reviewed Olivia’s spectral display with us. As shown in the image below, she experienced a decrease in slower Theta wave activity (4–7 Hz) and an increase in faster Alpha waves (8–12 Hz), which are closer to the desired SMR range. Alpha activity is also associated with a calming state.
By the end of her first session, Olivia had shown small but meaningful increases in SMR. She was making progress – yay!
What Is a Spectral Display?
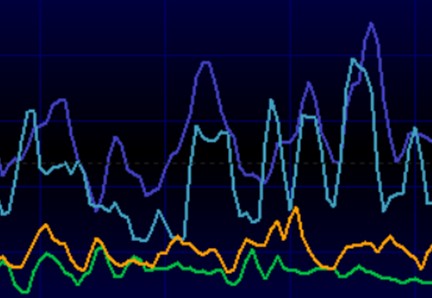
A spectral display shows the different brain waves occurring at a specific location in the brain.
In Olivia’s display above, you can see she had a higher amount of Theta activity (4–8 Hz), shown by the purple line. Theta is a slower brainwave rhythm. Her technician wanted to increase her SMR (12–15 Hz) activity instead, as SMR is associated with calming and improved movement control.
Research suggests that rewarding SMR activity over the sensory motor cortex (CZ) can help reduce movement issues. In the image below, the green line shows Olivia’s SMR activity at the beginning of her first session.
Beginning vs. End of Neurofeedback Session

Baseline Mean of SMR activity 6.91 (02.21.22.)

HRV Beginning vs End of 1st Session Data
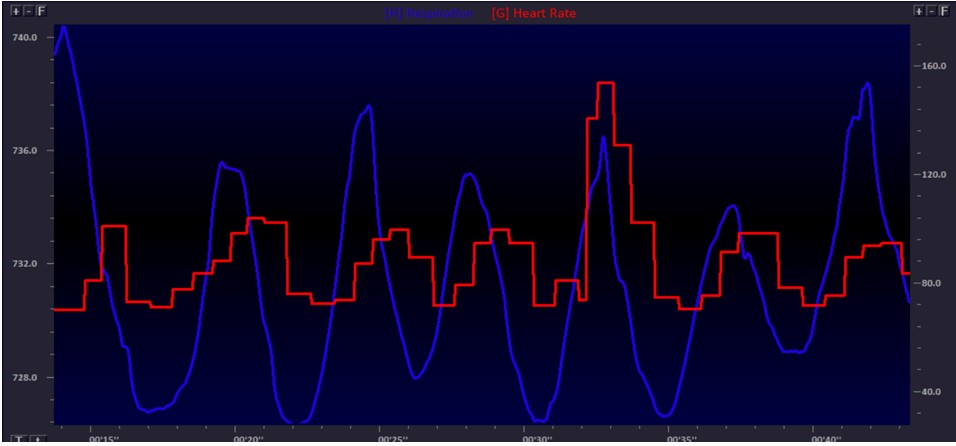
Beginning HRV
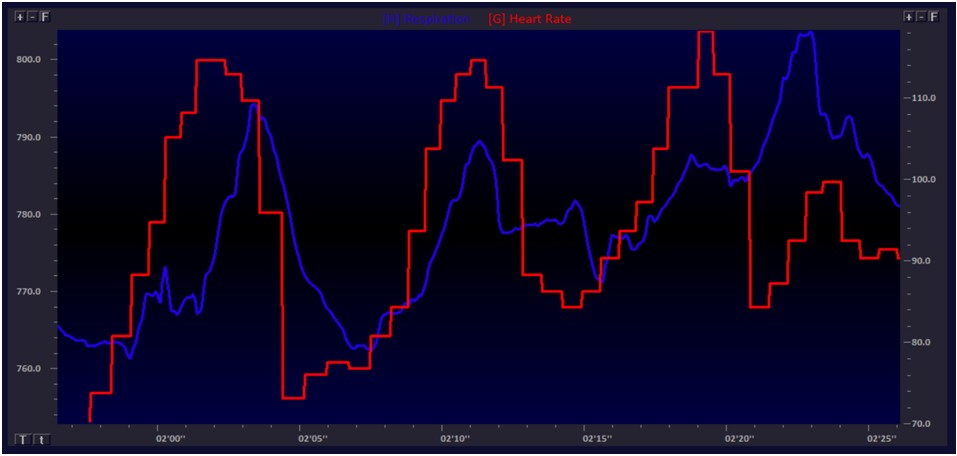
Ending HRV
HRV Biofeedback Results
During this part of the session, Olivia reached a breathing rate of 6.5 breaths per minute (BPM). Her biofeedback technician noted that she appeared calm and focused.
In the images above, you can see that as her breaths slowed (the blue line), they began to sync with her heart rhythm (the red line). This synchrony indicates she was entering a more optimal physiological state.
Achieving this “resonant frequency of breathing” helps the body recover more fully and function at its best.
The Massage Therapist
When we discovered that Olivia was experiencing extreme neck tension, we added massage therapy alongside her EMG biofeedback sessions. She loved getting massages, and they helped reduce her muscle tightness even further.
Asking Her Teacher
At the same time, I reached out to Olivia’s teacher to explain what was happening. Her teacher told me she had noticed the movements but reassured me that she hadn’t seen any other children making fun of her. That was a relief, though it was heartbreaking to think about.
I let her teacher and the school know that we would be taking Olivia out of class daily for her neurofeedback appointments. They were incredibly supportive of her treatment and our efforts to help her.
Typical Course of Treatment
Current treatments for movement disorders include botulinum toxin injections, deep brain stimulation (DBS), medications, and physical rehabilitation. Despite advances in these treatments, they still present significant limitations, such as undesirable side effects, limited effectiveness, and lack of specificity.
Typical Treatment for Movement Disorders – Medication
Medications can help manage some symptoms of movement disorders, depending on the condition. For example, patients with Parkinson’s disease are often prescribed medications to increase dopamine levels in the brain. While dopamine replacement medications can alleviate motor symptoms, other motor and non-motor symptoms often remain resistant. Long-term use of dopamine therapy can also lead to side effects such as impaired limb proprioception, dopamine dysregulation syndrome, and motor fluctuations.
Sources: Broccard et al., 2014. Annals of Biomedical Engineering. Temple Health Treatment Options
Does Neurofeedback Work as a Treatment for Movement Disorders?

Because movement disorders can have many different causes, it’s important to understand that not all tremors respond the same way to treatment. Most neurofeedback research on tremors has focused on the beta frequency band. One recent study found that reducing theta waves and stimulating the motor cortex through beta frequencies could decrease tremor amplitude.
Note: SMR (Sensory Motor Rhythm) activity includes part of the beta frequency range.
As traditional, more invasive therapies fall short in improving patients’ quality of life, new non-invasive approaches like neurofeedback are gaining attention. Neurofeedback teaches individuals to self-regulate targeted brain activity patterns, enhancing cognitive abilities and reducing clinical symptoms.
Using Neurofeedback to Improve Motor Skills
- Sensorimotor Rhythm (SMR) is one of the most promising EEG targets for enhancing motor skills.
- In stroke patients, SMR neurofeedback training has been used to reduce hypokinetic activity by downregulating mu rhythm or low beta SMR activity, enhancing motor control.
- In ADHD patients, SMR neurofeedback aims to reduce hyperkinetic activity by training the brain to upregulate low beta SMR activity during rest and attention tasks.


At Olivia’s next session, her neurofeedback technician reviewed the treatment plan and continued targeting SMR activity over her sensory motor cortex. Olivia didn’t seem to mind—she got to watch a fun movie during the training.
The technician explained that whenever the movie played, it meant Olivia was successfully shifting her brain activity into the desired range. At first, the movie kept pausing, but by the end of the session, it played with minimal interruption. When the technician asked Olivia how she made the movie play, she smiled and said she just tried to relax.
And so, her sessions continued from there.

Summary of Session
Olivia experienced minimal tics during this session. For the biofeedback portion, she completed three minutes of EMG training for her shoulders. During neurofeedback, she spent 30 minutes encouraging SMR activity at Cz.
Changes Starting and Continuing
After about five neurofeedback sessions, my husband and I both noticed a significant reduction in her tics. By session ten, Olivia went an entire day without a single tic!
I remember asking my husband what he thought. Each time, he looked uncomfortable and said, “It seems good so far, but I don’t want to say anything yet.” I’d ask, “Well, you’ve seen less, right?” He would respond, “I don’t want to get my hopes up.”
I understood. I felt the same way. Even though I knew what was happening—how neurofeedback works—it still felt almost too good to be true.
Olivia’s technician had targeted her sensory motor cortex. When she activated that area in the proper way, she was rewarded with the movie playing on the screen. In essence, she was exercising a new neuronal pathway, strengthening and enhancing the functioning of that part of her brain. This process was healing her brain, and as a result, her tics were reducing and eventually disappearing.
I knew all this in theory, but for my husband, seeing the actual results mattered more than any explanation.
In those early days, both of us watched her closely, biting our lips in anticipation, waiting to see a tic. If one appeared, we’d immediately text each other about it. But as the weeks went on and her tics became less and less frequent, we finally began to let go of that constant worry.
The Neurologist Appointment (After 10 Neurofeedback Sessions)
Finally, the neurology appointment arrived. My husband took Olivia while I waited anxiously to hear how it went. When he returned, he told me it was “short” and “unhelpful.”
The neurologist told him there was good news and bad news. The bad news was that they didn’t know why the tics had started or stopped. The good news was that since the tics were no longer present, we could leave his office.
I couldn’t believe it. Not only did he feel the tics didn’t need further investigation, but he also completely dismissed the fact that the only intervention we pursued—aside from paying multiple medical professionals for their opinions—was neurofeedback. It kills me to this day that he simply shrugged and said, “Well, maybe it worked, but I really can’t tell you. The tics are gone, so… you can go home now.”
My Experience in Video Form
A Few Months Later
After a while, we stopped thinking about the tics every day. My husband and I no longer felt anxious about them, and we got used to her not having them. But when I think back to those initial days and months, the fear returns – the fear that they might come back when she gets overly stressed or as her brain matures and prunes itself during puberty. For now, though, I am forever grateful for neurofeedback.
Olivia’s Treatment Continued…
Olivia began to show a few tics in the evenings during her first week of school in 2022. I wasn’t surprised; stressful times (and the first week of school is always stressful) can cause symptoms to resurface. My husband mentioned once or twice over the next few months that he noticed a tic or two. Although it freaked me out, I tried to just “keep an eye on it.”
I knew that 51 sessions wasn’t an “ideal” number and wanted her to complete at least 70, but I tried to put it out of my mind and wait. Then, in mid-November 2022, I started seeing them a bit more often and asked her about it. She said, “Mom, it’s fine. I like doing them.” I asked if she would go back to neurofeedback, and she said yes.
They weren’t daily or even weekly, but when I saw them, they were a bit more elaborate than just one simple movement, and I didn’t want to wait for them to worsen. During her Thanksgiving break, I took her back in for neurofeedback. 🙂


What is a “Booster Session?”
Clients often ask me, “How many neurofeedback sessions will I need?” That’s a difficult question to answer. Ideally, I recommend anywhere from 50 to 70 sessions to achieve optimal results.
I always caution clients not to stop neurofeedback too early, even if their symptoms improve after just 10–20 sessions. The brain needs time to solidify new neural networks, and stopping too soon can lead to symptoms re-emerging – often to a lesser extent, but returning nonetheless.
I also explain the idea of “booster sessions,” like I did for Olivia. When the brain is under stress (such as starting a new school year) or undergoing rapid changes (like during puberty), it’s not uncommon for symptoms to increase. Returning for neurofeedback booster sessions during these times can be incredibly helpful, even if only for a short duration.
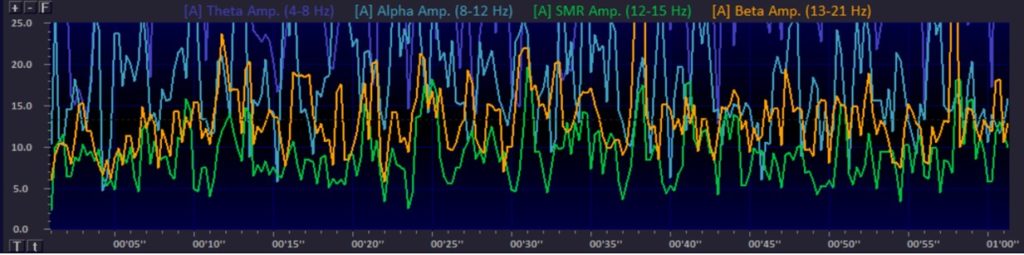 Baseline Mean of SMR activity (at the beginning of the session): 7.44 (11.23.22)
Baseline Mean of SMR activity (at the beginning of the session): 7.44 (11.23.22)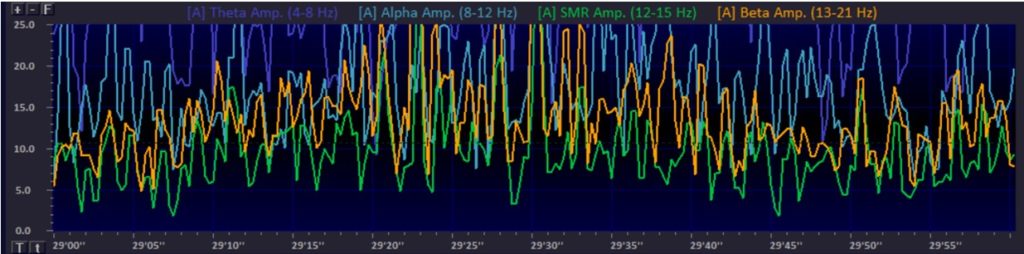
Summary of Session
During Thanksgiving break in 2022, we took the opportunity to have Olivia return for three combined biofeedback and neurofeedback sessions. After those sessions, her tics stopped again, so we decided to pause treatment for the time being.


